Minimally Invasive Keyhole Bunion Surgery
With over 98% success rate, The Bunion Surgeon is one of the leading minimally invasive keyhole bunion experts in the United Kingdom.

What are the benefits of minimally invasive keyhole bunion surgery?
The minimally invasive keyhole bunion operation has several benefits including:
- Reduced swelling following the bunion surgery
- Decreased postoperative pain
- Faster return to closed footwear and normal activities
- Smaller incision resulting in less visible scar
- Reduced chance of joint stiffness
What is Minimally Invasive Bunion Surgery?
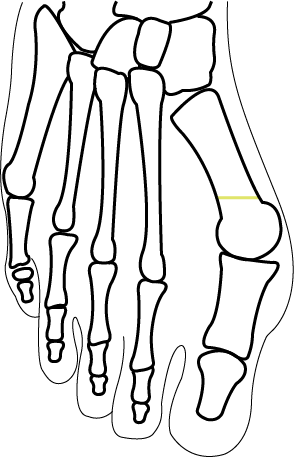
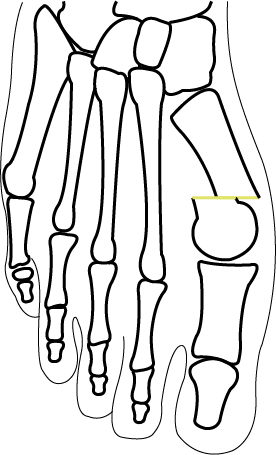
Keyhole bunion surgery, or minimally invasive bunion surgery, is a modern technique to surgically correct a bunion.
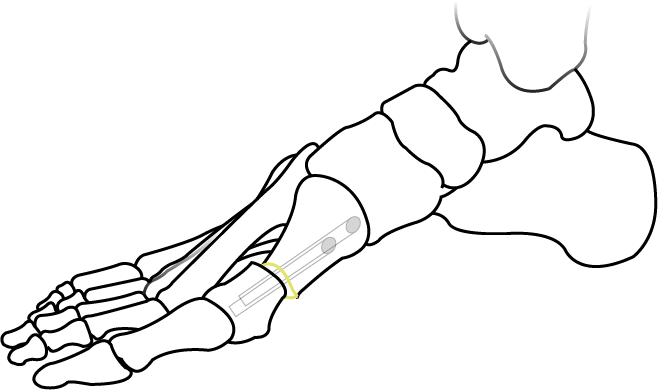
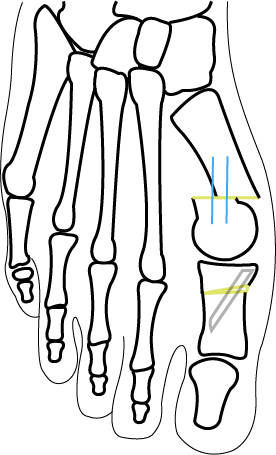
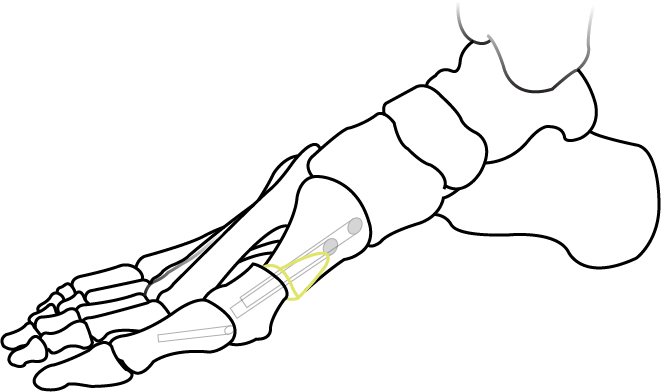
A live X-ray machine is utilised during the procedure to aid the cut and resetting of the bone malalignment using 3 to 4 small 1 to 3mm incisions to guide the specialised surgical instruments designed for bunion correction, that will fix the bones in the corrected position.
The area heals much quicker than more traditional bunion correction. This is due to minimal scar tissue.
Mr Kaser Nazir has seen excellent results with his patients who have reduced pain and quicker recovery.
How is the minimally invasive bunion procedure performed?
Minimally invasive surgery timeline
Why is a screw fixation required for the minimally invasive bunion correction?
Research shows that without a fixation keeping the joint in place once the bones have been realigned increases the risk of complication such as delayed or non union of bones and recurrence of the deformity.
Mr Kaser Nazir utilises the PECA correction system with screws that significantly reduces the chance of the bunion recurring and provides a predictable recovery.
This includes immediate weightbearing with minimal pain and swelling.
Frequently Asked Questions
Can you prevent Bunions?
Bunions can be prevented, or at least slowdown in terms of the progression, by using appropriate fitting and supportive footwear. A rigid-soled shoe with good support in the counter of the heel and some arch support can help prevention of bunions.
However, you are mostly predisposed to have developing the bunion due to genetics and therefore footwear alone may not be able to prevent bunions. Not wearing pointy shoes or high heels would reduce the risk of developing bunions even though you are predisposed to them.
Why are women more likely to develop a Bunion during pregnancy?
During the late stage of pregnancy the hormonal changes cause loosening of the ligaments and collagen in particular to allow for delivery of the baby. It is indiscriminate in the type of tissues that loosen and overall the ligaments around the foot can loosen resulting in flattening of the arch and widening of the forefoot. This results in the bunion worsening during the pregnancy period. Furthermore, the increased weight due to the baby will also place greater pressure on the feet and hence the bunion deformity can progress.
How do shoes cause a Bunion?
Whilst shoes alone are unlikely to cause bunion. We note that pointy shoes will result in pushing the big toe towards the second toe and therefore weaken the ligaments and thus cause the bunion deformities.
How do I know if I have a Bunion?
If you have a prominence of bone that feels hard on the inside of the big toe and feels lumpy then that is most likely to be a bunion. You will also note that the big toe will not be facing forwards but slanted towards the second toe even in mild cases.
Can men get Bunions?
Men and women are equally likely to get bunions. However, in Mr Nazir's experience, women wear slimmer and more pointy shoes that results in them seeking for medical attention much more than men.
Does wearing high heels cause Bunions?
High heels do place extra pressure on the front of the foot and can increase the likelihood of you developing a bunion deformity.
Why do you use screws in Bunion correction surgery?
Whilst the surgery to correct bunions can be performed without screws the evidence suggests that the chances of developing reoccurrence or long-term swelling increase. Movement of unstable bones creates more reaction from body and therefore the swelling increases.
In Mr Nazir's experience, the reoccurrence of the bunion deformity is also higher and the limitation of the degree of deformity that can be corrected is limited when screws are not used. Using screws will allow early weight bearing but also control swelling and allow accurate correction of the deformity. The screws are especially made for bunion surgery and do not irritate the skin and sit inside the bone and therefore do not cause irritation. They do not cross the joint and therefore do not cause joint stiffness which is a common misconception.
Is there no scar with minimally invasive bunion surgery?
The procedure does produce a small amount of scarring, but these are very small incisions that are used to correct the bunion deformity using minimally invasive or keyhole surgery. This is different to open surgery where a big incision is made and therefore the scar is more visible and the tissue can be more stiffer and cause problems.
Does Bunion correction surgery hurt?
Bunion correction surgery does involve an operation and most patients will only report a mild discomfort for three to five days. Some patients will get more pain for up to five to seven days and will require pain relief for that period. Surprisingly, the pain is very minimal following bunion surgery even though in the past it has had a bad reputation, especially with older open surgery techniques.
Can I have both Bunions treated at the same time?
Yes, Mr. Nazir treats many patients who require bunion surgery on both feet and would prefer to have the operation performed on both feet at the same time. This is not a problem with the modern minimally invasive keyhole bunion surgery techniques.
When can I wear heels after Bunion surgery?
A typical response to this is that at three months it is very likely that you can wear high heels following bunion surgery. Some patients can wear high heels after eight weeks but this very much depends on postoperative swelling and patient’s comfort.
Will I need physiotherapy after Bunion correction?
Most patients do not require physiotherapy following bunion surgery as the minimally invasive bunion surgery techniques are unlikely to cause joint stiffness. Occasionally patients have tenderness around the joint or increased swelling which is unusual that requires some deep tissue manipulation and massage and therefore a referral for physiotherapy is made.
When can you drive after minimally invasive bunion surgery?
Typically, if you are driving automatic car then you can drive with your left foot after a few days following the operation. However, if the right foot is operated on then the minimal period with minimally invasive is four weeks and can be up to six weeks following the operation, as you will need to be able to perform in emergencies. Otherwise, your insurance could be void.
Will my Bunion return after surgery?
The bunion deformity reoccurrence rates are less than 2% with modern bunion surgery techniques used at the clinic. Older techniques did have a higher rate and hence the repetition precedes.
Can I have Bunion surgery on the NHS?
Yes, bunion surgery can be performed on the NHS. However, you will need to speak to your GP and get a referral to your local NHS department and the exact technique will be dependent on the expertise of the surgeon.
Can you walk again after Bunion surgery?
There is no concern regarding not being able to walk or even run following bunion surgery provided there are no other concerns even prior to surgery and that you are fit and healthy and can perform these activities.
Are you awake for Bunion surgery?
This is very much the patient’s choice. Some patients decide to stay awake during Bunion surgery and others prefer to be sedated during the operation. Most patients have some sort of sedation with a local anaesthetic.
What is a Hammertoe?
A hammer toe is the deformity of the second toe where you get flexion deformity and retraction of the toes, so that causes the toe to rub against shoes. It is a complication of bunion deformity and hence patients with bunion surgery often present with a second hammer toe deformity.
Can you have surgery to correct a Hammertoe?
The surgery to correct the hammer toe can also be performed using minimally invasive technique. Mr. Nazir specialises in minimally invasive hammer toe correction.
Can you treat a Bunion and a Hammertoe at the same time?
Yes, both bunion and hammer toe surgeries can be performed at the same time. The deformities can co-exist. There is no increased recovery time or increased discomfort or limitations if the surgery is performed at the same time. Contact our team for further information or to request a quote.
When is the best time for Bunion treatment?
Bunion treatment should start when you have difficulty with footwear fitting or developing pain. If you are having the deformity of the second toe develop due to the bunion deformity and the second toe becomes painful, then that is also an indication to consider treatment.
Is finance available for minimally invasive keyhole bunion surgery?
Mr. Nazir or his clinic does not directly deal with finance as we try to provide the best service possible and deal with clinical care mostly. However, The Weymouth Street Hospital do provide payment plans for bunion surgery. Following a consultation we can introduce you to the hospital as needed. Please enquire.
What is the total cost of minimally invasive keyhole Bunion surgery?
The clinic provides fixed cost surgery which includes the surgery and anaesthetic fees and hospital fees as well as any equipment that is to be required during the operation. All postoperative visits are also included. Visit out pricing page for further information on bunion surgery fees.
Can Bunions cause osteoarthritis?
Long-standing bunion deformity of the big toe can cause osteoarthritis of the joint due to the joint being partly dislocated. This causes cartilage wear and hence the arthritis in the joint.
Where can I have Bunion removal near me?
You will need to speak to your GP or look at local hospitals where bunion surgery is provided. Mr. Nazir provides the service mainly in Central London and has a typical waiting list of one to three months.
If you do have your treatment with Mr. Nazir then you will be required to attend for surgery and postoperative follow-up at least six weeks following surgery in London, where X-rays will be carried out to assess bone healing. The rest of the appointments can be arranged locally for you or remotely as needed.
When can you start to exercise after minimally invasive bunion surgery?
You can do non-weight bearing exercises after one week, which would involve sit ups and crunches.
You can use a static bike about four weeks post bunion surgery with minimally invasive surgery.
Running mostly to be commenced between 6-8 weeks depending on the procedure and healing.
When can you swim after minimally invasive bunion surgery?
Typically, the wound will heal over a two-week period, however most patients will be able to swim after three weeks once the wound has consolidated a little more. You will be able to get your foot wet after two weeks, but swimming, which would involve long periods of water immersion, is possible at three weeks.